What is Visual Snow Syndrome?
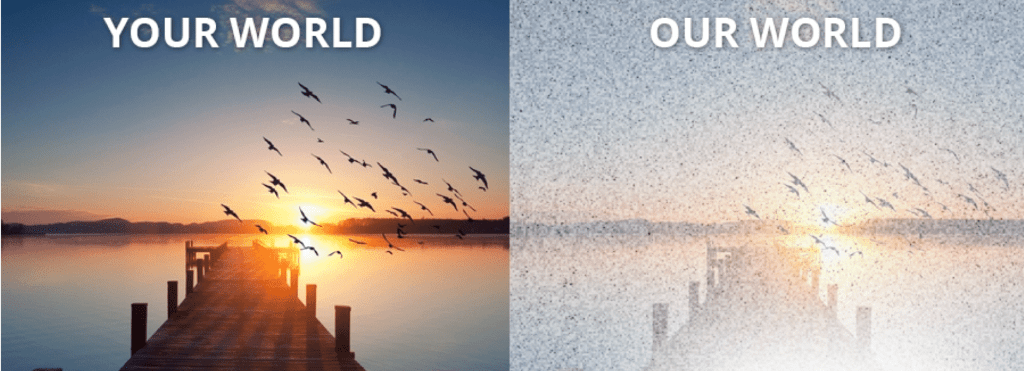
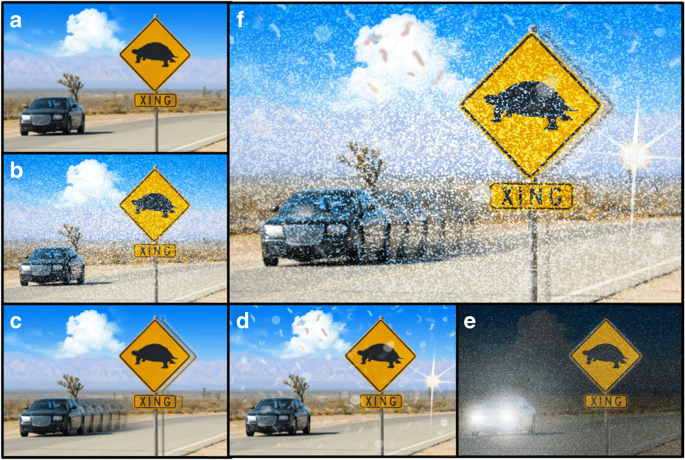
Visual Snow Syndrome (VSS) is a neurological condition that affects vision, hearing, cognition, sensory processing, and overall quality of life. It is characterized by persistent visual disturbances, such as constant “visual snow” or static, flickering dots, and flashing lights visible 24/7 with eyes open and closed. Beyond its hallmark symptom, VSS includes a range of non-visual issues as well. Originating in the brain, VSS is classified as a network brain disorder, meaning it impacts multiple interconnected brain regions, including those responsible for vision. This dysfunction, marked by hyperactivity in some areas and reduced connectivity in others, disrupts sensory information processing and contributes to its wide array of symptoms. The impact of VSS on quality of life varies from mild to debilitating and affects an estimated 2-3% of the global population. The condition can be present from birth or develop at any stage of life.
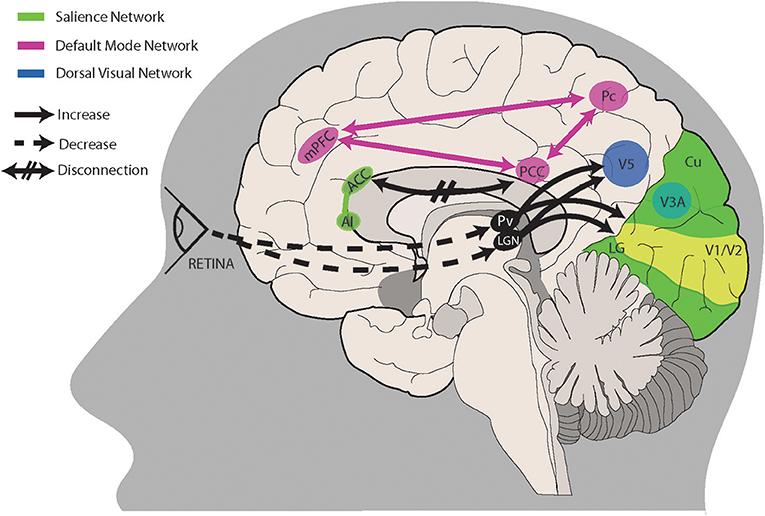
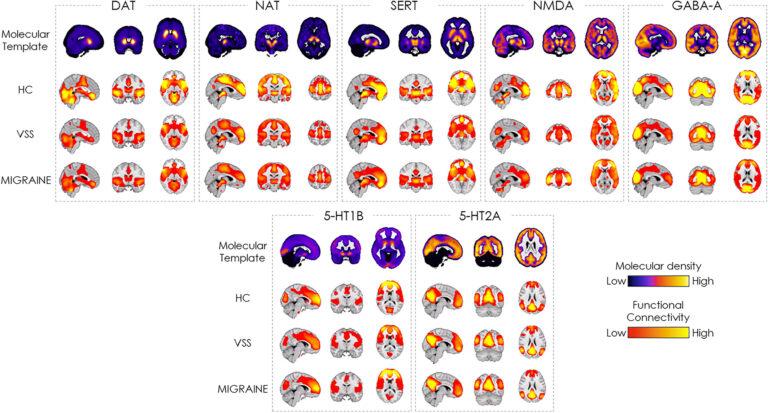
VSS is now recognized as a legitimate and distinct network brain disorder caused by disruptions in interconnected neural pathways. It involves both hyperactive regions, like the visual cortex, and downregulated areas, such as the anterior cingulate cortex, which explains the condition’s complexity and the variability of symptoms among individuals. Recent research has identified abnormalities in glutamate and serotonin neurotransmitter networks as potential biomarkers, with advanced imaging techniques like 7-Tesla MRI and PET scans providing insights into these disruptions. Importantly, VSS is not a manifestation of anxiety or depression; rather, its debilitating nature, compounded by historic misdiagnoses and marginalization, can severely impact mental health. As medical and scientific recognition of VSS grows, continued advocacy, education, and research are essential to improving diagnosis, treatment development, and support for those affected, with the ultimate goal of finding a cure.
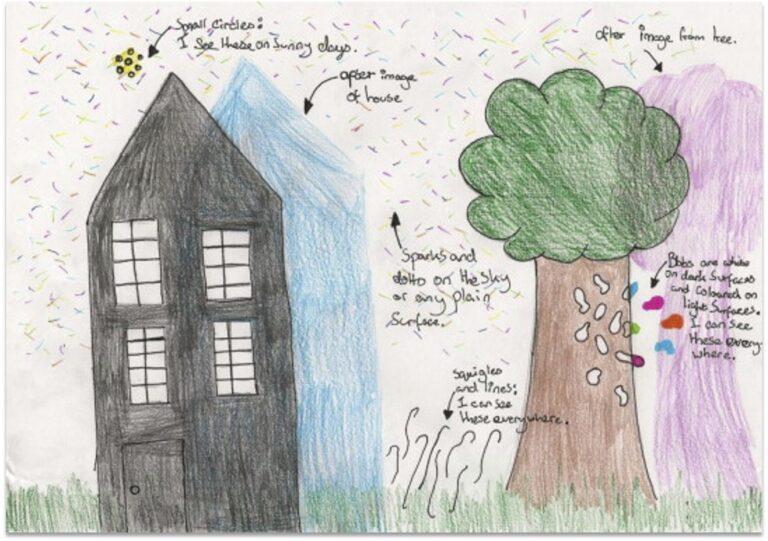
Drawing by 12 year-old girl with Visual Snow Syndrome
Simpson JC, Goadsby PJ, Prabhakar P. Positive Persistent Visual Symptoms (Visual Snow) Presenting as a Migraine Variant in a 12-year-old girl. Pediatr Neurol. 2013;49:361-3.
What Are the Symptoms of Visual Snow Syndrome?
The primary symptom of Visual Snow Syndrome (VSS) is seeing visual snow, which can be described as seeing static, flickering dots, and flashing lights 24/7 (with your eyes open and closed). Some describe it as trying to see in the middle of a snowstorm or through a snow globe that has been shaken up. However, VSS entails more than just seeing visual snow. People with VSS also commonly experience many other debilitating visual and non-visual symptoms, such as palinopsia, photophobia, tinnitus, paresthesia, anxiety, depression, depersonalization, and insomnia. The intensity, appearance, and degree of impact of these symptoms range from mild to moderate to life-altering, depending on the person.
Please use the following link to access our Diagnostic Criteria for Visual Snow Syndrome (to share with your doctor, etc.), as well as a more comprehensive list of symptoms with photo references.
What Causes Visual Snow Syndrome?
Visual Snow Syndrome (VSS) is a network brain disorder, meaning it results from disruptions in the interconnected neural networks of the brain rather than being confined to a single area. These networks are responsible for coordinating sensory, motor, and cognitive processes, and when they become dysregulated, it can lead to the wide range of symptoms observed in VSS.
Network Dysfunction and Complexity
Research shows that VSS involves both hyperactive and downregulated areas in the brain. For example, the visual cortex (particularly the lingual gyrus) and thalamus, which play key roles in processing and filtering sensory input, are often hyperexcitable. At the same time, other brain regions show reduced activity or connectivity. This combination explains why VSS symptoms are so varied and why the condition affects individuals differently. These disruptions in neural networks create persistent visual disturbances, such as static, and can extend to non-visual symptoms, including tinnitus, migraines, and sensory overload.
Potential Triggers and Onset
While the exact cause of VSS is still unknown, patients have reported a wide variety of potential triggers for the onset of symptoms. These include:
- Certain medications, particularly those with serotonin reuptake inhibiting properties, as demonstrated in clinical research
- Episodes of extreme physical or mental stress
- Concussions or traumatic brain injuries (TBI)
- Migraines, including migraine with aura
- Infectious diseases
- Surgical procedures
The diversity of these potential triggers highlights the complexity of the condition and suggests that VSS is affected by a combination of genetic, neurological, and environmental factors.
Possible Biological Markers
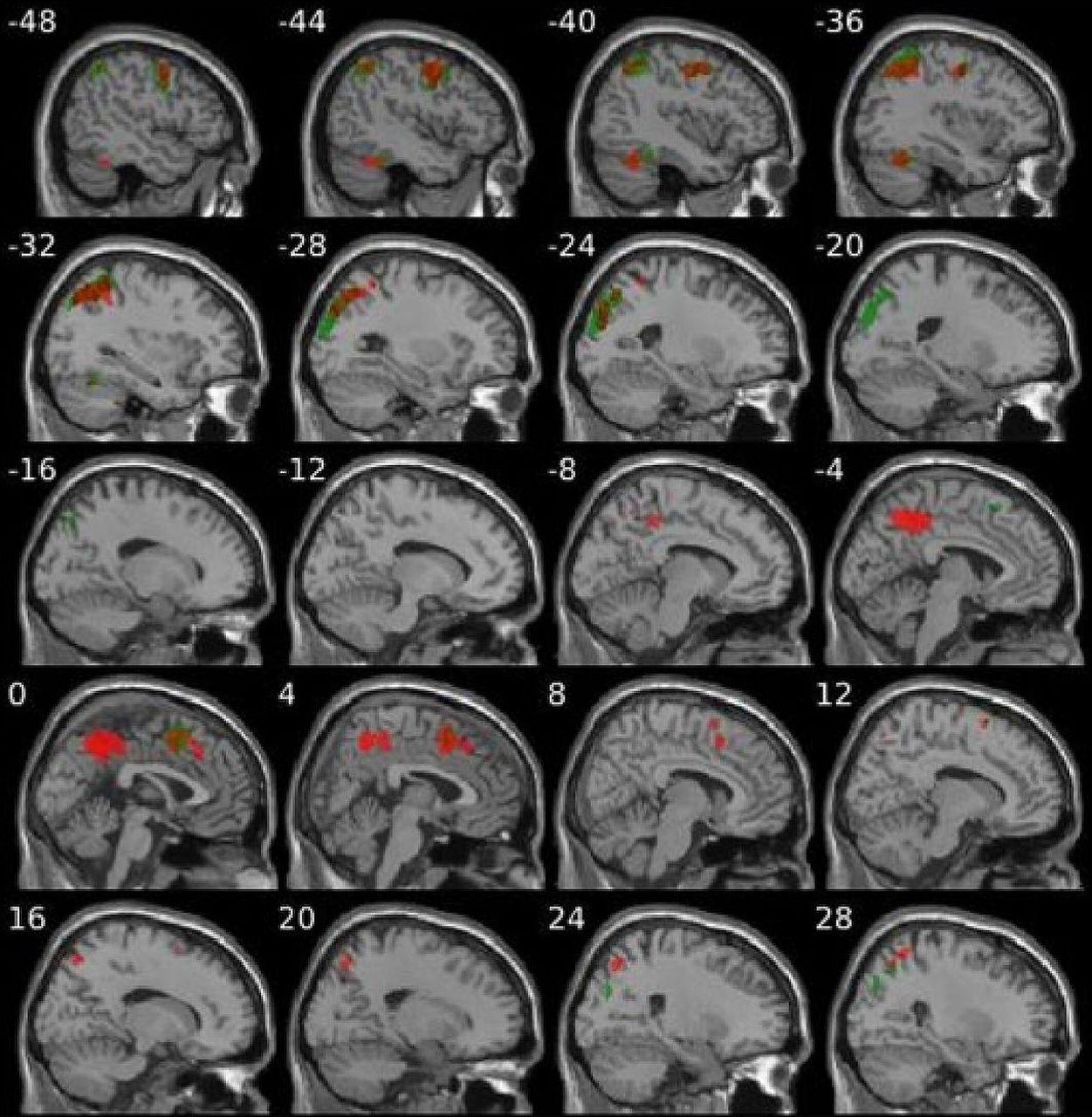
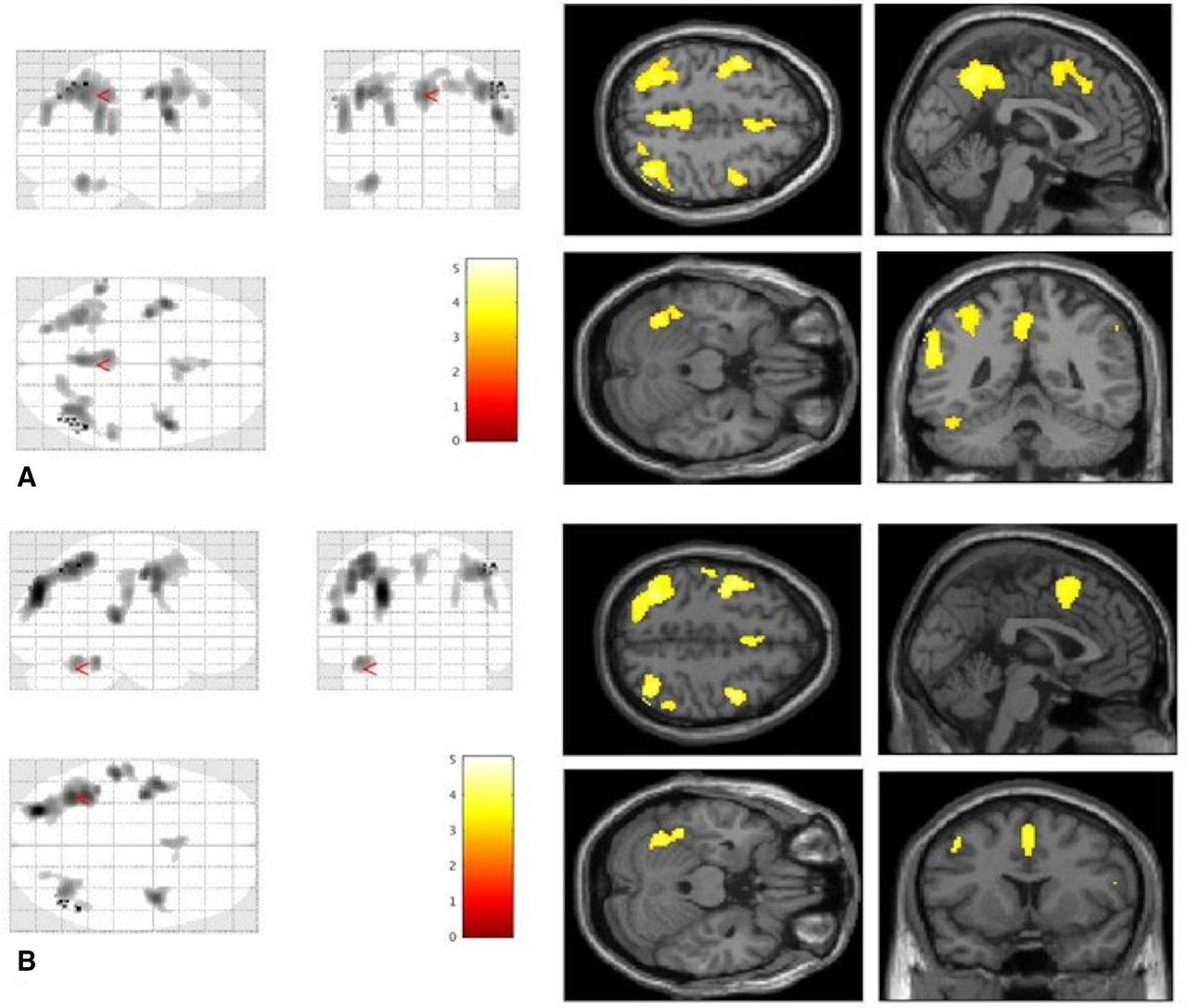
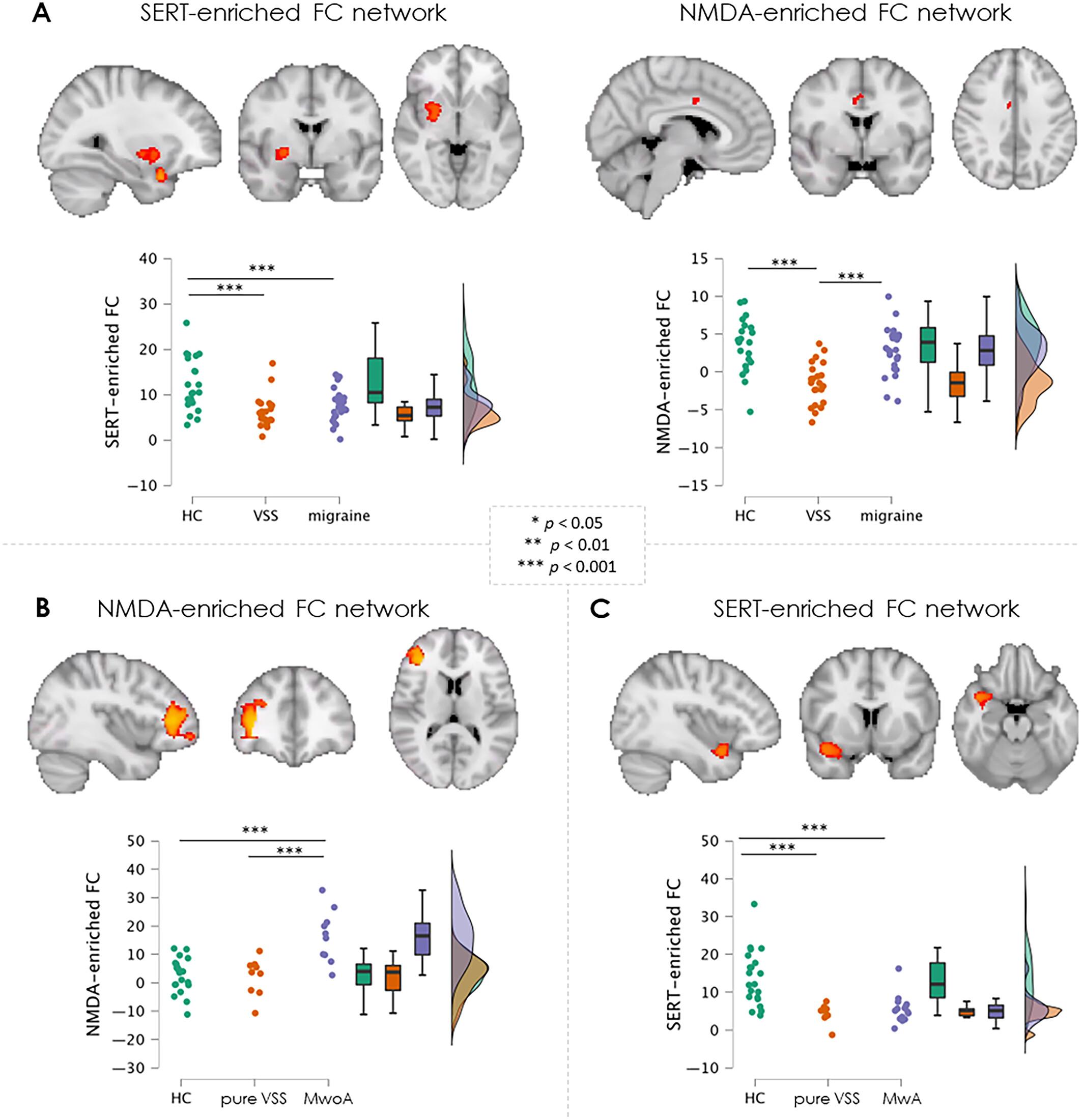
Recent groundbreaking studies funded by Visual Snow Initiative have uncovered possible biomarkers for VSS, revealing abnormalities in two key brain chemical systems: glutamate and serotonin. Using advanced imaging techniques, researchers have identified differences in the activity of these neurotransmitter systems in individuals with VSS compared to healthy controls.
- Glutamate Networks: Reduced functional connectivity in the anterior cingulate cortex (ACC), a region responsible for integrating and filtering sensory information, suggests a disruption in how the brain processes visual input.
- Serotonin Networks: Reduced connectivity in areas like the visual cortex, insula, temporal pole, and orbitofrontal cortex may influence the integration of complex sensory information. This pattern of serotonin activity also links VSS to conditions such as migraine with aura.
These findings highlight how the interplay between hyperexcitable and downregulated brain areas contributes to the complexity of VSS and its wide-ranging symptoms.
Advanced Imaging Insights
Studies utilizing 7-Tesla MRI and FDG-PET/MRI have also revealed microstructural and functional connectivity differences in cortical and thalamic regions in individuals with VSS. By combining PET imaging with functional MRI through a technique called Receptor-Enriched Analysis of Functional Connectivity by Targets (REACT), researchers have created detailed maps of brain chemical activity, offering new insights into the biological basis of VSS.
Ongoing Research and Progress
Research into the causes and mechanisms of VSS is advancing rapidly. While significant progress has been made in identifying the underlying brain network disruptions, potential triggers, and biomarkers, the exact origins of VSS remain unknown. Efforts to better understand its pathophysiology continue to grow, providing hope for additional targeted treatments in the future.
Latest News & Research on Visual Snow Syndrome
Here, our team will share the latest news and updates regarding the Visual Snow Initiative, research studies, interviews, projects, as well as any additional information related to our global efforts to better understand, treat, and/or cure Visual Snow Syndrome.
How Do You Diagnose & Treat Visual Snow Syndrome?
Historically, receiving an accurate diagnosis for Visual Snow Syndrome (VSS) has been challenging. Diagnosis is based on a patient’s symptoms and a thorough clinical evaluation, including a detailed medical history and a comprehensive eye exam to rule out eye-related conditions. It is common for optometric and ophthalmological exams to yield “normal” results in VSS patients. In some cases, additional testing, such as an MRI or EEG, may be ordered to rule out other neurological conditions. VSS is typically diagnosed as a condition of exclusion, requiring the patient to meet specific diagnostic criteria.
Medical professionals best equipped to address VSS include neuro-ophthalmologists and neurologists, as well as some ophthalmologists, optometrists, neuro-optometrists, and vision therapists trained in managing VSS symptoms. Depending on the patient’s specific symptoms and medical history, managing VSS often requires a multidisciplinary approach. Physicians specializing in neurological and/or ocular aspects of the condition may work together to develop a comprehensive, individualized treatment plan.
Types of Physicians Who Treat VSS
- Neuro-ophthalmologist: Specializes in visual issues linked to the nervous system, combining expertise in neurology and ophthalmology
- Neurologist: Diagnoses and treats disorders of the brain, spinal cord, and nervous system
- Ophthalmologist: Focuses on eye care, including diagnosing eye conditions and performing surgeries.
- Neuro-optometrist: Combines neurology and optometry to address vision problems related to neurological conditions
- Optometrist: Provides eye exams, prescribes corrective lenses, and manages common eye conditions
Since VSS is a neurological disorder that affects sensory processing, particularly the interaction between the brain and the visual system, diagnostic and management efforts must address both visual and non-visual symptoms. Neurologists may perform exams and imaging studies to evaluate brain function, while ophthalmologists and optometrists may assess eye health and visual function. Collaboration between these specialists can improve diagnostic accuracy and treatment outcomes.
If you suspect you have VSS, refer your doctor to the Diagnostic Criteria provided by Visual Snow Initiative (VSI). Although it can be challenging to find professionals familiar with VSS, VSI offers a directory of physicians and specialists worldwide who have expertise in diagnosing and managing the condition. For more information, visit our Doctors & Specialists Directory.
As more awareness is raised about VSS, medical professionals with expertise in treating related symptoms within their practice are better equipped to help patients manage this complex condition. Through communication, collaboration, and specialized care, individuals with VSS can receive tailored support and effective symptom management plans.


Support Visual Snow Syndrome Research
All donations to the Visual Snow Initiative go directly to Visual Snow Syndrome (VSS) research.
Your tax-deductible contribution ensures that global research will continue and makes a positive difference in the lives of people affected by VSS.