Researchers
Eliseo Barral, Elisa Martins Silva, David García-Azorín, Michele Viana and Francesca Puledda
Abstract
Migraine is a severe and common primary headache disorder, characterized by pain as well as a plethora of non-painful symptoms. Among these, visual phenomena have long been known to be associated with migraine, to the point where they can constitute a hallmark of the disease itself. In this review we focus on two key visual disorders that are directly or indirectly connected to migraine: visual aura and visual snow syndrome (VSS). Visual aura is characterized by the transient presence of positive and negative visual symptoms, before, during or outside of a migraine attack. VSS is a novel stand-alone phenomenon which has been shown to be comorbid with migraine. We discuss key clinical features of the two disorders, including pathophysiological mechanisms, their differential diagnoses and best treatment practices. Our aim is to provide an aid for clinicians and researchers in recognizing these common visual phenomena, which can even appear simultaneously in patients with an underlying migraine biology.
Introduction
Migraine is a prevalent neurological disorder, listed by the Global Burden of Disease Study as the second leading cause of years lived with disability worldwide [1]. It affects around 15% of the general population globally and is typically characterised by recurring, highly disabling attacks of severe head pain lasting for 4–72 h, associated with nausea, vomiting, increased sensitivity to light and sound and numerous neurological signs and symptoms [2]. The diagnosis of migraine is clinical and based on criteria provided in the third edition of the International Classification of Headache Disorders (ICHD-3) [3]. Migraine being a primary headache, individuals will typically have a normal physical examination with no underlying causes for their pain [3,4]. However, migraine is much more than a disorder of head pain, and alteration of vision as a neurological dysfunction symbolises one of the hallmarks of the disease. In fact, up to a third of patients may experience transient focal neurological symptoms in at least some of their attacks which fulfil the diagnostic criteria for the condition of migraine with aura (MwA) [5].
Visual disorders are also a common feature of migraine outside of the context of aura. Some patients, for example, can experience transient visual disturbances during the migraine attack lasting only a few seconds and over the bilateral visual field [9]. Further, some patients with migraine biology seem to be predominantly affected by the migraine-associated phenomenon of visual snow [10].
This narrative review has the purpose of examining the main clinical features of typical and atypical visual aura, the newly described phenomenon of visual snow and associated syndrome, and to aid the clinician in the differential diagnosis between these disorders. A brief overview is also given of known pathophysiological mechanisms of these two distinct but related conditions, as well as current treatment options.
Visual Snow Syndrome
3.1. History and Clinical Features of Visual Snow Syndrome
Visual snow (VS) is an entity first described in a case series in 1995 by Liu et [35], as an ‘unusual complication of migraine’, while the term used to describe it was introduced a decade later [36]. The clinical criteria of visual snow syndrome (VSS) were defined by Schankin and Goadsby [37,38].
Being an underrecognized disorder, VSS has often been misdiagnosed, with possible attributions varying from functional neurological disease to persistent aura. The stereotypic descriptions of the syndrome and the recent research on its pathophysiology, however, show unique brain changes leading to a distinctive dysfunctional central sensory processing [39]. The high comorbidity with migraine [40], as well as aura, further suggests a shared pathophysiology among these disorders [37]. Some authors have also suggested VSS may only represent an ‘exceptionally heightened awareness’ of physiological visual phenomena [41], but this view disregards the burden and efforts to manage this condition [42]. In fact, visual snow syndrome (VSS) presents with varying levels of disability and may strongly impact the quality of life of its sufferers [43].
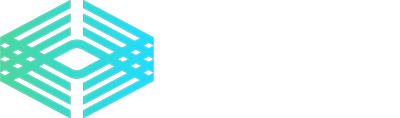
The ‘snow’ or ‘static’ in VS is described as a persistent and dynamic visual disturbance, characterized by numerous tiny flickering dots, similar to a detuned television. These are more frequently black and white (black/grey on a white background or grey/white on a black background) but can also be transparent or coloured. Although the snow is typically continuous [44], it can infrequently occur in an episodic fashion, either during migraine attacks or before the onset of a classic VSS form [45,46,47]. Episodes described in the literature range from a minimum of two minutes to the entire duration of a migraine attack. Prospective symptom recording on a diary in over one-hundred patients with VSS showed that visual static is quite steady over time [48]. A prospective longitudinal study conducted on seventy-eight VSS patients showed that the condition did not change for nearly a decade in most cases (80%) and no patient, over a mean of 7 years, went into spontaneous complete remission [44].
In the full visual snow syndrome, other visual and non-visual symptoms are present, making the condition more severe [43]. The typical additional symptoms are as follows: palinopsia, enhanced entoptic phenomena (which include excessive floaters in both eyes, excessive blue field entoptic phenomenon, self-lighting of the eye and spontaneous photopsia), photophobia, and nyctalopia. Palinopsia is characterized by positive afterimages that can be illusory or hallucinatory [19]. The latter are very realistic, previously seen images, occurring with no external stimulus, frequently with concomitant visual field defects, and should warrant caution as they can be related to structural disease. In illusory palinopsia the primary image suffers a distortion, it is not as clear as the first real image and is more influenced by ambient conditions. [49] This falls into the dysfunction of visual perception which occurs in VSS.
Due to symptoms such as nyctalopia and photophobia, VSS can largely impact daily life activities, such as driving at night, reading, and using screens [50]. Further symptoms that have previously been reported but that are not included in the definition of VSS are: ‘straight lines moving across the visual field’, ‘water running down a window’ and kaleidoscopes of colours even with eyes open [38]. Some authors have proposed inclusion of these in the clinical criteria, as ‘other persistent positive visual phenomena’ [51].
With regards to demographics, a recent population-based study showed the prevalence of VSS to be between 1.4% and 3.3% [41]. This study included participants unaware of the specific topic of investigation and who did not seek medical attention for their symptoms, therefore implying that a proportion of this population was not affected by symptoms in their day-to-day life [52]. VSS also shows phenotypic homogeneity across geographical areas [53].
The disorder usually starts in early life, and there seems to be no gender imbalance, much unlike migraine [43]. Nevertheless, women report higher intensity of VSS symptoms [50]. Approximately 40% of patients report symptoms for as long as they can remember, and triggers for symptom onset are often unidentifiable [43,53]. In a recent retrospective case series, however, around 40% of patients developed VS. abruptly after a perceived inciting event. Traumatic brain injury (TBI) was the most frequent of these, with VS occurring in concomitance with daily headaches and post-concussive symptoms [45]. With no optimal therapeutic approach currently available, primary cases of visual snow tend to remain stable over time.
Environmental factors that worsen visual snow are manifold, including low-light conditions, harsh artificial light, bright sunlight, and darkness [50]. Indoor and fluorescent lights may have a worse effect on symptoms when compared with natural outdoor lighting [48]. Frequently reported individual factors related to worsening include the following: fatigue, anxiety, alcohol consumption, inadequate sleep, exercise, caffeine, and screen use [45,50].
Aside from the frequent association with migraine, VSS patients often experience the non-visual sensory symptom of tinnitus (up to 70% of VSS cases [43]), usually described as high-pitched and continuous. Both migraine and tinnitus have been independently associated with a more severe presentation of VSS [43]. Patients might also experience somatosensory symptoms, or even tremor and balance problems [54]. Psychiatric comorbidity—with symptoms such as anxiety, depression, depersonalization, fatigue, poor sleep—is also common and further impacts quality of life. Depersonalisation, in particular, relates to increased severity of VSS symptoms and seems to be an intrinsic characteristic of the disorder rather than secondary to the disability caused by the symptoms [50].
3.3 Differential Diagnosis of VSS
Diagnosis of VSS requires a careful neuro-ophthalmic history and a thorough investigation of the visual pathway. It has in fact been shown that, although the syndrome is generally benign and primary, it may occasionally present as secondary to other causes [45]. Identifying an inciting event is relevant since these are potentially treatable and tend to have better prognosis compared to spontaneously occurring VSS. Hang et al. suggest some red flags when evaluating possible VSS, including: new-onset visual snow, onset at an older age, intermittent or sudden exacerbation of VS, unilateral or hemifield VS, absence of additional visual disturbances, history of recently discontinued illicit drugs, and additional visual or neurologic changes [68].
Different ancillary exams can be used to exclude secondary causes, but there are no standard guidelines. Vaphiades et al. suggest that for those patients reporting a typical VSS history with normal neuro-ophthalmologic examination, including automated perimetry, other ancillary testing may be unnecessary [69]. Sampatakakis et al. recommend a brain MRI and EEG in all VSS patients with palinopsia, the most common additional symptom, which, as described above, can be associated with potentially severe conditions [52]. The differential diagnosis of visual snow, particularly when onset is rapid, should include bilateral optic neuropathies, such as metanol intoxication, ischemia, Leber optic neuropathy, and folate or B12 deficiency.
Hallucinogen persisting perception disorder (HPPD) can manifest in the visual snow spectrum [43]. This condition is described in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition [70] as a re-experiencing of perceptual symptoms, usually visual, and felt during intoxication with a hallucinogenic drug. In HPPD the visual symptoms, which often resemble visual snow, can be unremitting; they can occur with different recreational drugs, including cannabis, ecstasy, lysergic acid diethylamide, and psylocibin [71]. Van Dongen and colleagues studied the association between VSS with migraine and VSS with HPPD, showing that these are phenotypically distinct populations [72]. They hypothesized that HPPD had a different initiation mechanism with respect to ‘primary’ VSS. Both conditions, however, lack good therapeutic options [71].
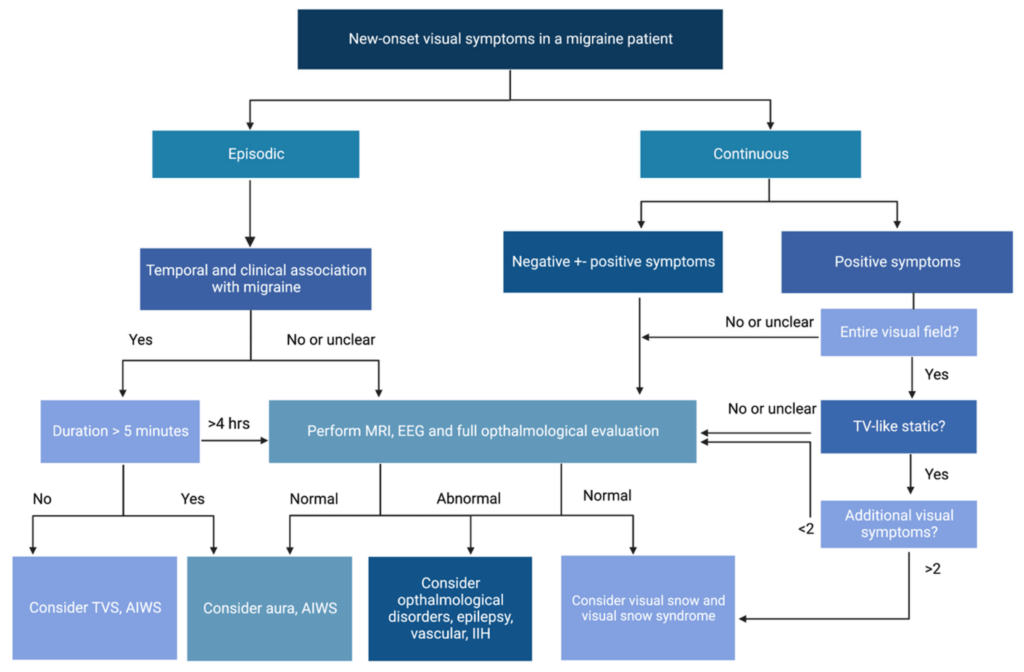
Finally, as detailed in Table 1, visual snow can be present episodically among the classic visual disturbances of aura, so particular attention should be made in patients who have a background of migraine and a history of visual and non-visual aura in order to appropriately distinguish the two conditions (Figure 2). A diagnostic algorithm for visual disturbances associated with migraine is shown in Figure 3.