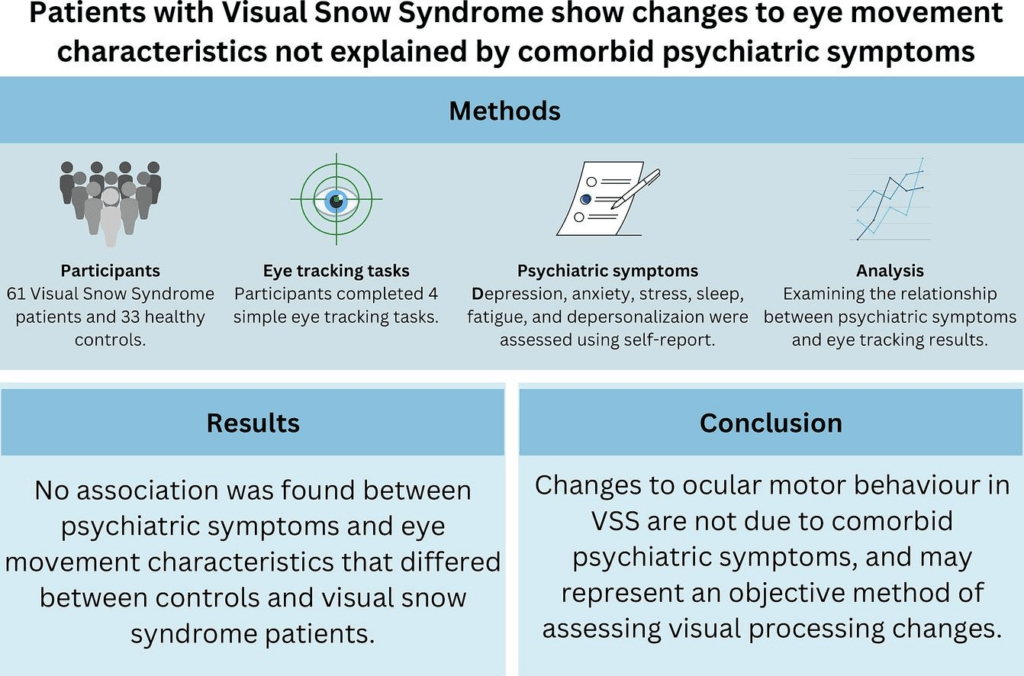
This 2023 study by the Visual Snow Initiative is significant as it provided scientific evidence consistent with previous research, further proving that Visual Snow Syndrome (VSS) is a distinct neurological condition, not a psychiatric disorder.
This is important because, historically, individuals with VSS have been met with skepticism by the medical community, often dismissed as “imagining” their symptoms, labeled as “crazy,” or mistreated—despite VSS always being a legitimate neurological condition.
According to the study, if VSS were psychiatric in nature, symptoms like anxiety or depression would be expected to impact eye movement patterns. However, the study found no significant influence, confirming that neurological mechanisms drive VSS. This aligns with established research indicating that VSS results from abnormal sensory processing in the brain, rather than from psychiatric illness, thereby giving VSS validity as a legitimate neurological condition.
Abstract
Visual snow syndrome (VSS) is a neurological disorder primarily affecting the processing of visual information. Using ocular motor (OM) tasks, we previously demonstrated that participants with VSS exhibit altered saccade profiles consistent with visual attention impairments. We subsequently proposed that OM assessments may provide an objective measure of dysfunction in these individuals.
However, VSS participants also frequently report significant psychiatric symptoms. Given that that these symptoms have been shown previously to influence performance on OM tasks, the objective of this study was to investigate whether psychiatric symptoms (specifically: depression, anxiety, fatigue, sleep difficulties, and depersonalization) influence the OM metrics found to differ in VSS. Sixty-one VSS participants completed a battery of four OM tasks and a series of online questionnaires assessing psychiatric symptomology.
We revealed no significant relationship between psychiatric symptoms and OM metrics on any of the tasks, demonstrating that in participants with VSS, differences in OM behaviour are a feature of the disorder. This supports the utility of OM assessment in characterising deficit in VSS, whether supporting a diagnosis or monitoring future treatment efficacy.
Introduction
Visual snow (VS) is a persistent positive visual disturbance across the entire visual field, with the co-occurrence of at least two additional visual symptoms supporting a diagnosis of visual snow syndrome (VSS) (The International Classification of Headache Disorders, 2013). At present, the aetiology of VSS is unknown and there are no objective clinical markers of the disorder.
Recently, we demonstrated that ocular motor (OM) measures provide a method of assessing visual processing changes in the disorder, providing a potential marker of dysfunction that can be used to aid diagnosis and monitor any future treatment outcomes. Although we found that migraine, a frequent VSS comorbidity, did not impact our OM measures, it remains unclear whether the varied and common comorbid psychiatric symptoms of VSS (depression, anxiety, poor sleep quality, fatigue, and experiences of depersonalization/derealization) do impact performance, as has been reported in other populations.
We demonstrated previously that individuals with VSS reorient gaze to a suddenly appearing target more quickly than neurologically healthy individuals (i.e., make faster latency prosaccades). VSS participants also exhibit greater difficulty withholding a response to non-target stimuli (i.e., increased antisaccade errors) or when attention is endogenously cued to non-target location (increased inhibitory errors on tasks endogenously manipulating attention). However, these studies did not consider the numerous psychiatric symptoms that are common in VSS.
VSS cohorts consistently report mood (39 %) and anxiety (45 %) disorders, and we have also shown that they frequently experience fatigue (50 %), poor sleep quality (45 %), and experiences of dissociation (specifically depersonalization/derealization, 27 %). Depression has been linked previously with slower saccadic latencies and increased inhibitory errors, and individuals with high levels of anxiety have been reported to generate slower antisaccades. Both sleep deprivation and fatigue have been associated with increased inhibitory errors and/or alterations to saccade latencies. Depersonalization and derealization have not been specifically investigated using OM tasks, but are known to involve attentional changes (Adler et al., 2014) which, given the inextricable link between attention and OM control could theoretically impact OM behaviour.
The aim of this study, therefore, was to determine whether depression, anxiety, fatigue, sleep deprivation, and depersonalization/derealization in VSS participants significantly influence OM task performance in these individuals.